Ichiro Maruyama
Graduated Japan Shiatsu College in 2012
Abstract : This report examines the case of a patient diagnosed with traumatic cervical spinal cord injury and suspected peripheral neuropathy (flaccid paralysis of the lower extremities) who was treated with shiatsu therapy for the alleviation of dorsal muscle tension. After 29 treatments, lower-limb motor function recovered. This suggests that hypertonicity in paraspinal muscles was significantly related to the motor dysfunction due to peripheral neuropathy. Considering other reports on the effect of shiatsu stimulation in improvement of muscle pliability, we conclude that in this patient the decrease in muscle hypertonicity due to shiatsu therapy resulted in improved blood circulation and increased spinal range of motion, leading to a recovery of motor function.
Keywords: flaccid paralysis of the lower extremities, shiatsu therapy, dorsal muscle tension
I.Introduction
Spinal cord injury refers to injury of the spinal cord where it is protected within the spinal canal. Depending on the level of the spinal cord injury, symptoms presented may include motor, respiratory, circulatory, urinary, digestive, or other dysfunctions. Treatment is divided between initial phase treatment and chronic phase treatment, with initial phase treatment including pharmacotherapy, localized rest, cranial traction, and surgery, while chronic phase treatment centers on rehabilitation. Here, we report on a case in which the symptoms of a patient diagnosed with traumatic cervical spinal cord injury virtually disappeared following therapy.
Ⅱ.Methods
Location
Patient’s home
Period
August 25 to December 1, 2014 (Number of treatments: 29)
Test subject
82 year old female
History of present illness
The patient sustained a traumatic cervical spinal cord injury 46 years previously. Rehabilitation restored motor function in the upper limbs, but paralysis (paraplegia) of the lower limbs remained and she had been confined to a wheelchair ever since. Six years previously she sustained a fracture to her right humerus, and later required amputation of the arm due to pyogenic osteomyelitis. Two years previously she was diagnosed with tuberculosis and admitted to a tuberculosis ward, after which she became bedridden. After discharge from the hospital, she developed pain in her upper limb and dorsal regions, and it was arranged for her to received homecare massage for alleviation of the pain.
Medical history
Paraplegia (circulatory organ, urinary, and digestive organ dysfunction) due to spinal cord injury; gallbladder cancer; pancreatic cancer; tuberculosis; amputation of right arm due to pyogenic osteomyelitis
Treatment
- Shiatsu to cervical, dorsal, sacral, and gluteal regions in lateral position
- Shiatsu to left upper limb and lower limbs in supine position (emphasis on treatment of lower limbs)
Evaluation
- Pain evaluated using 10-step VAS
- Manual muscle testing (MMT)
III.Results
August 25 (Treatment #1)
Pre-treatment findings
Subjective findings
- Motor paralysis and sensory dysfunction inferior to lumbar region
- Numbness below knees
- Bladder and rectal dysfunction
- Pain in upper limb and dorsal regions
- Hot and cold flashes (excessive sweating from neck up)
Objective findings
- Limited range of motion in left shoulder joint
- Flaccid paralysis and sensory dysfunction of lower limbs
- Pain in dorsal and gluteal regions
Post-treatment findings
- Hot and cold flashes alleviated due to improved circulation
- Pain reduced
September 4 (Treatment #4)
Post-treatment findings
- Dorsal region muscle tension reduced (thoracolumbar junction)
- Pain in medial femoral region absent
- Slight return of sensory function in femoral region (femoral nerve, obturator nerve)
- Muscle contraction observed in femoralregion (adductor muscles)
September 8 (Treatment #5)
Post-treatment findings
- Plantar pain absent
- Patient found shiatsu to sacral region pleasurable
September 18 (Treatment #8)
Post-treatment findings
- Patient felt urinary and bowel sensations (improvement of bladder and rectal dysfunction)
- Return of sensory function to femoral region
October 2 (Treatment #12)
Post-treatment findings
- Muscle contraction observed in femoral region (femoral nerve, obturator nerve)
October 30 (Treatment #20)
Post-treatment findings
- Muscle contraction observed in femoral region (sciatic nerve)
November 6 (Treatment #22)
Post-treatment findings
- Movement observed in hip joint (flexion, extension, external rotation, internal rotation)
- Movement observed in knee joint (flexion, extension)
- Left shoulder joint more stable; pain absent
- Changed sensation distal to knee
November 17 (Treatment #25)
Post-treatment findings
- Movement observed in ankle joint and toes (flexion, extension) with patient lying in lateral position
- Patient able to form slight bridge (elevation of gluteal region)
December 1 (Treatment #29)
Post-treatment findings
Subjective findings
- Patient experiences numbness in calcaneal region
- Pain eliminated
Objective findings
- Return of motor function inferior to lumbar region
- Improvement to bladder and rectal dysfunction
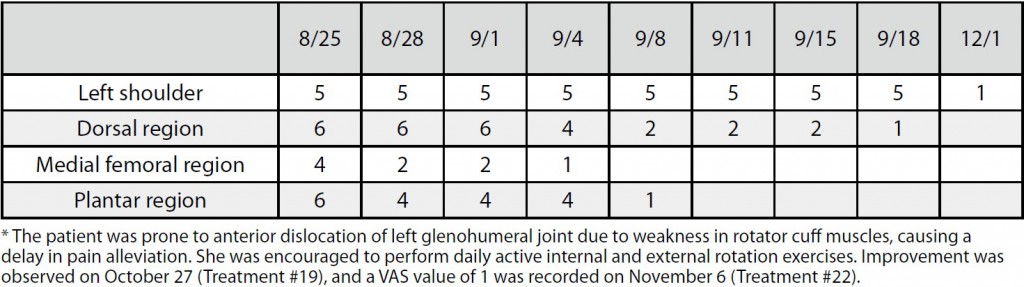
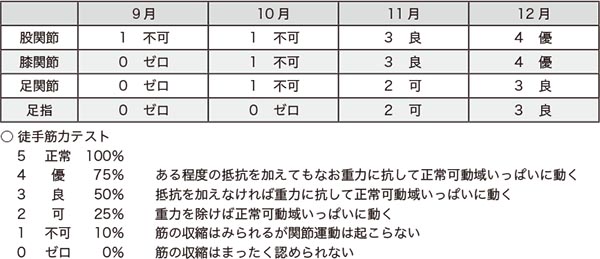
Table 1. 10-step VAS pain scale values (post-treatment)
Table 2. Manual muscle testing (MMT) of lower limbs
IV.Discussion
In most cases of spinal cord injury, the vertebrae undergo dislocation fracture due to an external force, with concomitant damage to the spinal cord. Characteristics vary depending on the level and degree of spinal cord injury (complete or incomplete paralysis), but immediately after the injury spinal shock occurs and autonomy is lost in the spinal cord inferior to the injury. Specifically, flaccid paralysis occurs, with loss of all motor, sensory, and deep tendon reflex function, while at the same time autonomic nervous function is also impaired. Following the recovery period, reflex functions in the spinal cord inferior to the injury are recovered, resulting in spastic paralysis, characterized by hyperreflexia of the deep tendon reflexes 1.
In this case, since the patient exhibited flaccid paralysis from post-injury to the present, it is likely that this was a case not of spinal cord injury, but rather of spinal cord compression. In other words, assuming lower motor neuron damage and comparing spinal cord injury level with ADL levels, since T1 ADLs (upper limbs normal, full wheelchair mobility) were possible and T6 functions (circulatory organ stability) were unstable, it was determined that there was an irregularity in the upper thoracic vertebrae. Clinical findings indicated that the thoracic spine was straight, with almost no curve in the thoracic vertebrae. We may hypothesize that this caused hypertonus in the dorsal musculature, causing lower motor neuron damage, pain, and motor dysfunction.
Based on the above determination of peripheral neuropathy due to spinal cord compression, shiatsu therapy was carried out with the objective of alleviating pain and restoring motor function in the patient. As a result, after 29 treatments, decrease in VAS values as an indicator of pain (Table 1) and recovery of muscle strength as determined by manual muscle testing (Table 2) were observed, although numbness remained in the calcaneal region. If this were a case of spinal cord injury, such rapid return of function would be unlikely 2-3. It is therefore reasonable to assume that recovery was due to shiatsu treatment of peripheral neuropathy caused by nerve entrapment due to hypertonic muscles.
At the very least, in this case it is highly likely that hypertonicity in paraspinal muscles was significantly related to the motor dysfunction due to peripheral neuropathy. Considering other reports on the effect of shiatsu stimulation in improvement of muscle pliability 4~6, we conclude that in this patient the decrease in muscle hypertonicity due to shiatsu therapy resulted in improved blood circulation and increased spinal range of motion, leading to a recovery of motor function.
V.Conclusion
Even in patients afflicted by long-term peripheral neuropathy (pain and motor dysfunction), recovery through shiatsu therapy is possible.
VI.References
1. Nara N et al: Toyo ryoho gakko kyokai rinsho igakukakuron (dai 2 han) sekizui sonsho. Ishiyaku shuppan KK: 171-173, 2010 (in Japanese)
2. Shinno Y: Massho shinkei shogai no rihabiriteshon. Nihon rihabiriteshon igakukaishi 28 (6): 453-458 (in Japanese)
3. Nishiwaki K et al: Massho shinkei sonshogo no shinkeisaisei to rihabiriteshon. Nihon rihabiriteshon igakukaishi 39 (5): 257-266, 2002 (in Japanese)
4. Asai S et al: Effects of Shiatsu Stimulation on Muscle Pliability. Toyo ryoho gakko kyokai gakkaishi (25): 125-129, 2001 (in Japanese)
5. Sugata N et al: Effects of Shiatsu Stimulation on Muscle Pliability(Part2). Toyo ryoho gakko kyokai gakkaishi (26): 35-39, 2002 (in Japanese)
6. Eto T et al: Effects of Shiatsu Stimulation on Muscle Pliability(Part3). Toyo ryoho gakko kyokai gakkaishi (27): 97-100, 2003 (in Japanese)