Shinpei Oki
Representative, Nekonote Shiatsu
Abstract : This report examines the case of a female patient in her 20s who received three full body shiatsu treatments between May 24 and June 7 2015, with the objective of reducing psychological stress. The psychological effect was evaluated using the Profile of Mood States (POMS) index. Following treatment, improvements in the t-scores of all six POMS factors were observed. This suggests that full body shiatsu therapy has a stress-relief effect, which may be verified through further studies.
Keywords: shiatsu, stress, POMS
I.Introduction
So many people are feeling the effects of psychological stress in modern society that stress can be considered endemic 1. In Japan, many people look to alternative therapies, including anma, massage, and shiatsu, for treatment of stress.
Multiple studies have been conducted into the effects of manual therapy on stress relief 2~5, confirming its effectiveness. Research has also been conducted into the use of shiatsu for treating stress 6, but insufficient data exists on the effects of general shiatsu carried out by a therapist on a patient. In this paper, we report on a case in which full body shiatsu used to alleviate stress with psychological stress measured using a mood profile, which will serve as a springboard for future investigation.
Ⅱ.Methods
Test subject
Female office worker in her 20s
Period
May 24 to June 7, 2015 (3 sessions)
Location
Patient’s home
Treatment method
Namikoshi-style full body shiatsu, starting in lateral position
Evaluation method
In order to evaluate psychological effects, a Japanese-language POMS™ test (Kaneko Shobo) was administered immediately before and after treatment. POMS is a mood profile test developed by McNair et al in the U.S., which employs answers to 65 questions to enable simultaneous measurement of six factors: tension-anxiety, depression, anger-hostility, vigor, fatigue, and confusion 7. The POMS results for this report were converted from raw data to t-scores and totaled. POMS has been implemented on large groups of healthy adult males and females and standardized, with t-scores calculated for mean value and standard deviation by age and sex. The t-score is calculated as 50 + 10 x (raw score – average score) / standard deviation. If the raw score is equal to the average score, the t-score will be 50. The lower the t-score, the lower the tension-anxiety, depression, anger-hostility, vigor, fatigue, or confusion. Thus, for vigor, a higher t-score indicates a more favorable condition 7.
The goal and measurement procedure for POMS was fully explained to the patient and her consent obtained.
Ⅲ.Results
History of present illness
The patient was transferred to a new department at work in April 2015 and, still unaccustomed to the new workplace and job responsibilities, was experiencing high daily stress levels. Work mainly involved VDT (video display terminal) operation, with over 7 hours per day spent engaging in computer input.
Medical history
Inguinal hernia (surgery completed in 2013)
Family history
No relevant items
Subjective findings
- Sleep disorder
On some days, the patient had difficulty getting to sleep because she was unable to relax emotionally. The harder she tried to sleep, the more difficult it would become. - Neck, shoulder, and lumbar pain
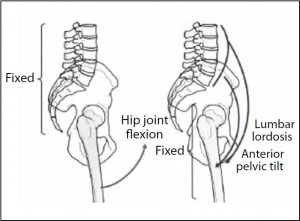
The patient experienced chronic neck and shoulder stiffness. Perhaps because she assumed the same posture for extended periods, she experienced a grinding pain when she extended her back.
Examination findings
- Observation
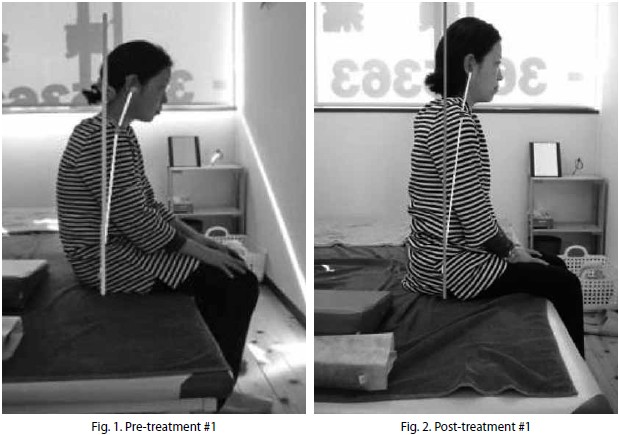
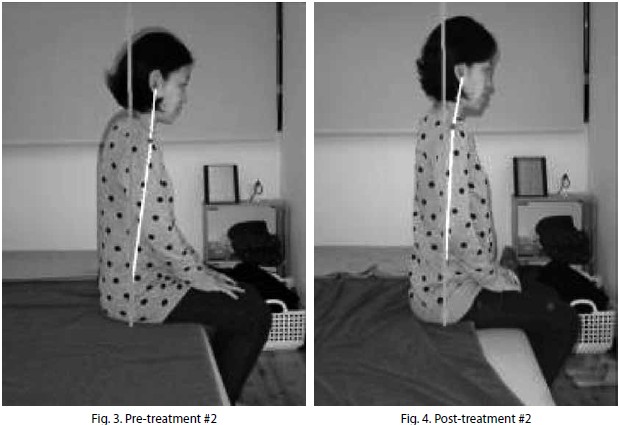
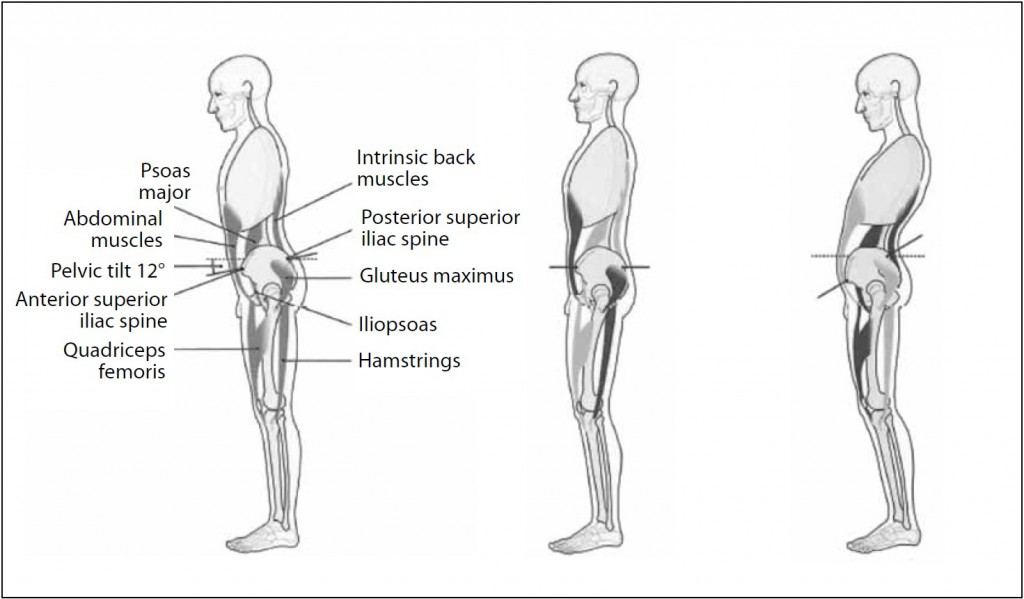
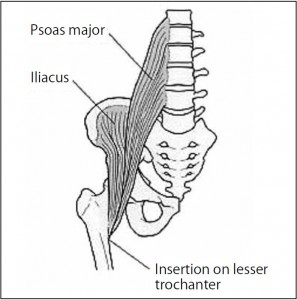
The patient’s complexion was poor, with bags under her eyes and numerous pimples around her jaw. Head-forward poster with exaggerated lumbar kyphosis was observed. - Palpation
Cervical region: Hypertonus was confirmed in anterior and middle scalenus, splenius capitis, rectus capitis posterior major and minor, and semispinalis capitis. Misalignment of the lower cervical vertebrae was also observed.
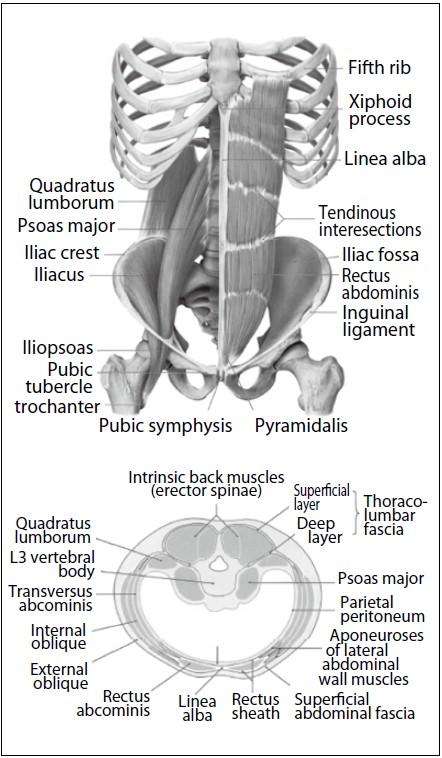
Shoulder, dorsal, and lumbar regions: Hypertonus was confirmed in the upper trapezius, levator scapulae, and quadratus lumborum.
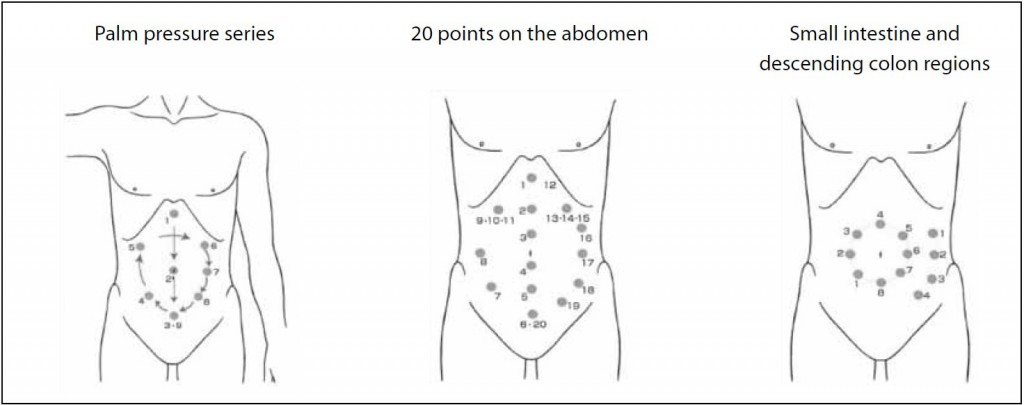
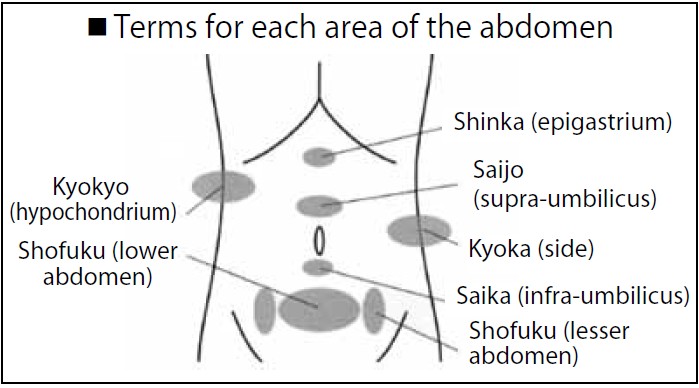
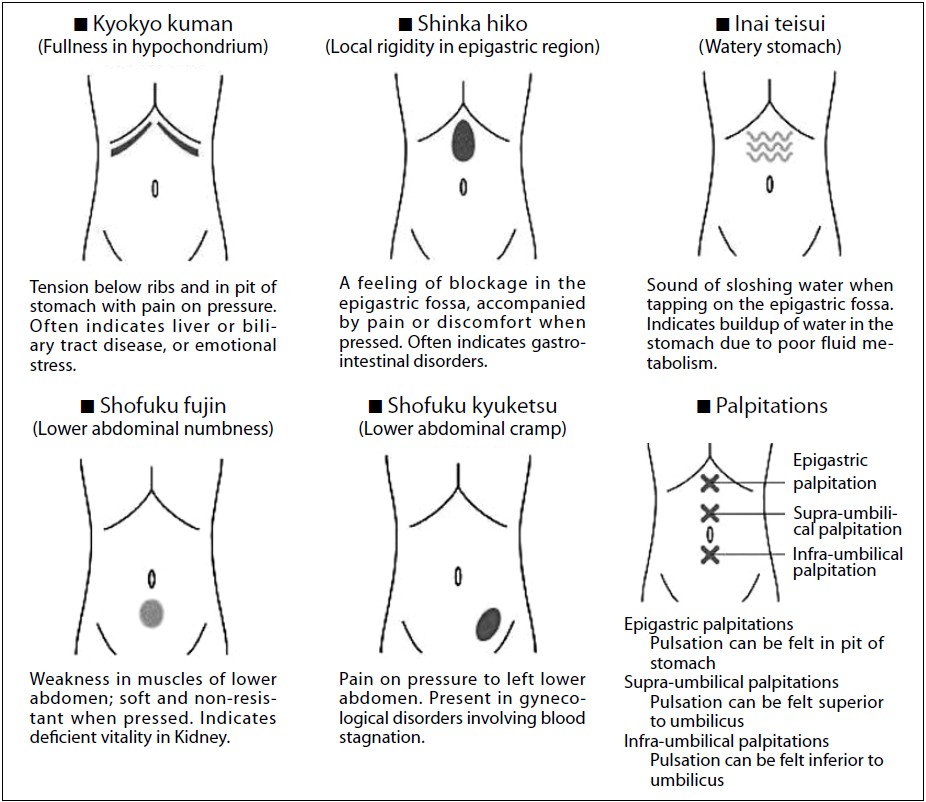
Abdomen: The lower abdomen was flaccid and induration was observed in the descending colon region (left umbilical region).
Treatment #1 (May 24, 2015)
- Rigidity in the dorsal region was alleviated.
- Post-treatment, the patient reported fullbody relaxation and mild drowsiness.
Treatment #2 (May 30, 2015)
- Patient reported that she slept well after the previous treatment and that she awoke the next morning with no feelings of lethargy.
- She also stated that her neck and shoulders felt lighter than usual.
Treatment #3 (June 7, 2015)
- Patient reported that she slept well for several days after treatment and that she felt comparatively fresh on waking.
- She still felt stiffness in the neck and shoulders, but it was not severe. Her lumbar region was still slightly stiff, but not painfully so.
- She felt that her stress level was lower as well.
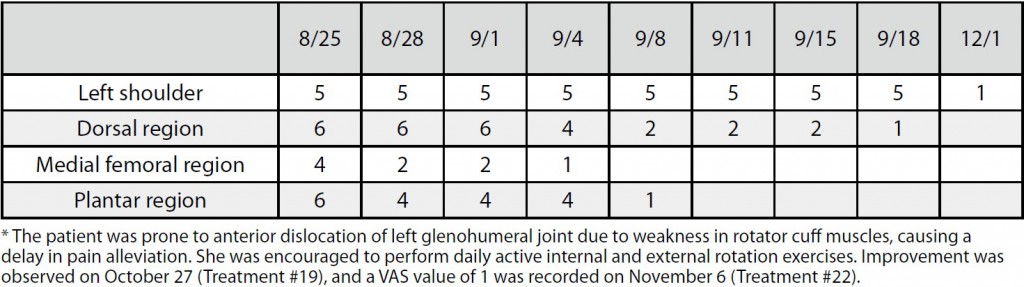
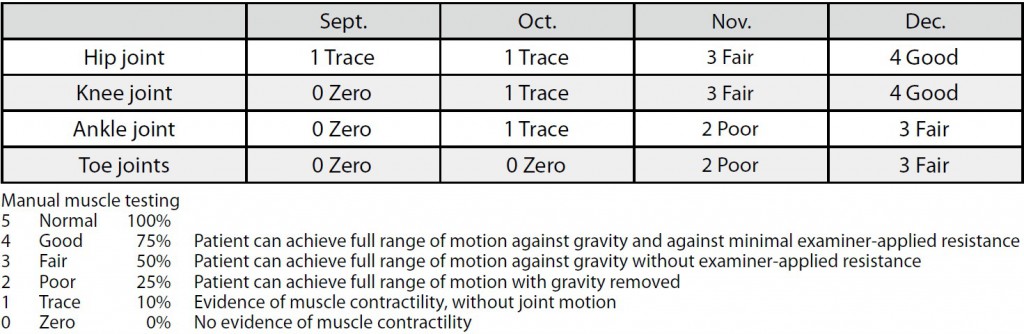
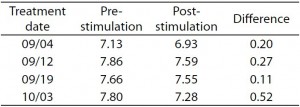
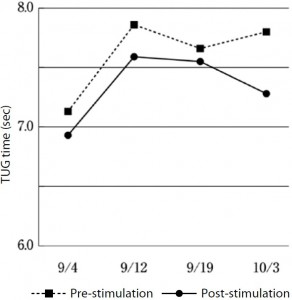
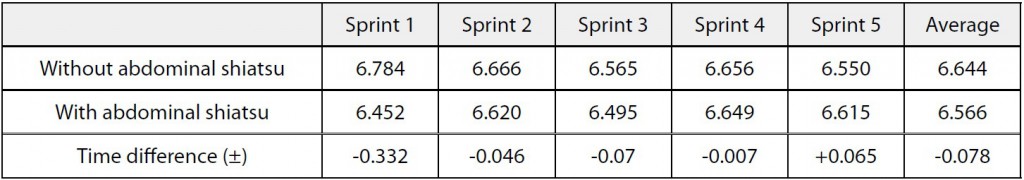
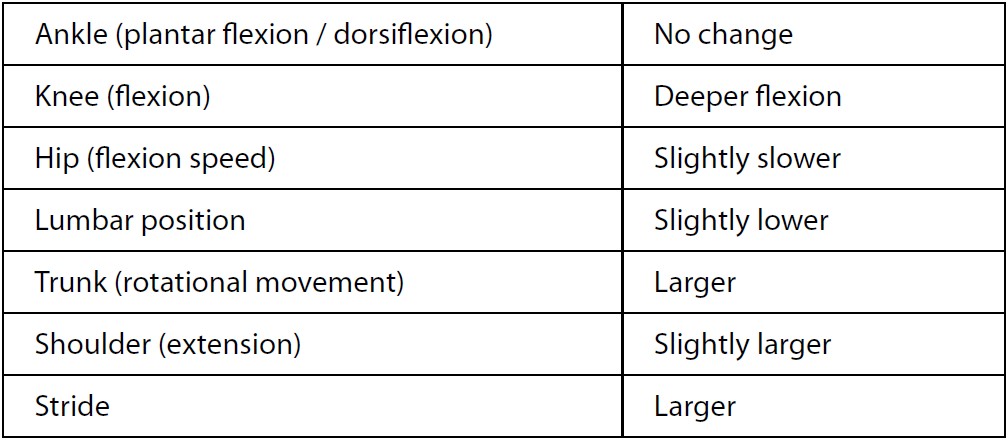
Table 1 shows the POMS t-scores measured before and after all three treatments. Aside from the anxiety factor on May 24 and the vigor factor on May 30, the values for all factors showed improvement posttreatment, with a general trend toward improvement as the treatments progressed (Fig. 1).
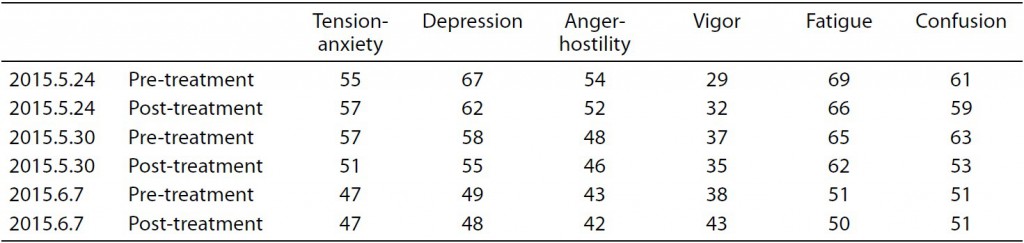
Table 1. T-scores for six POMS factors
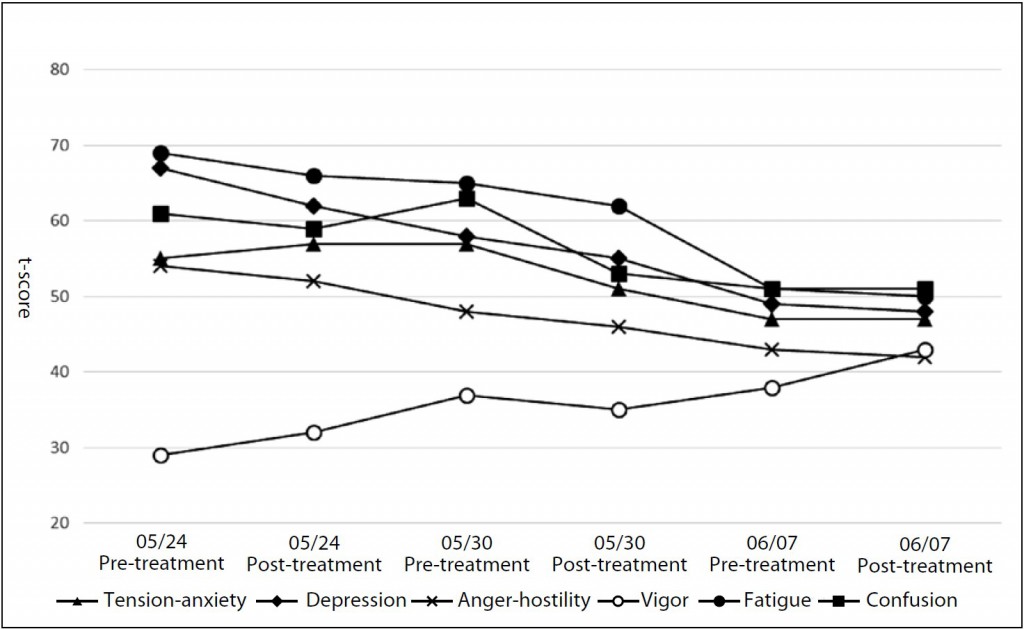
Fig. 1. Changes in t-scores for six POMS factors
Ⅳ.Discussion
In the case presented in this report, the patient showed improvement in all six POMS factors over the course of three treatments. Kamohara et al and Asai et al demonstrated the possibility for suppression of sympathetic nervous system activity using shiatsu to the abdominal region and the dorsal region, respectively 8-9. Also, Yokota, Watanabe, and Tadaka et al reported miotic (pupil contraction) response to shiatsu to the anterior cervical, lower leg, sacral, and head regions, respectively, possibly due to either suppression of the sympathetic nervous system or stimulation of the parasympathetic nervous system 10~12. The patient in this case report received full body shiatsu, including comprehensive shiatsu stimulation to all of the above-mentioned regions, so it is probable that a relaxation effect was achieved due to both suppression of the sympathetic nervous system and stimulation of the parasympathetic nervous system. In addition, Kato reported that, in restraint-stressed rats, acupuncture electrostimulation lead to normalization of secretion of monamines including dopamine and serotonin in all areas of the brain 13, so one might consider the possibility that a similar mechanism occurs with shiatsu stimulation as well.
A single case such as this is insufficient evidence to argue for the effectiveness of shiatsu therapy for treatment of stress. Verification of the effectiveness of shiatsu as a means of stress alleviation will require a study employing statistical methodology, which I hope to pursue as a research topic in the future.
Ⅴ.Conclusion
Improvement was observed in all six POMS factors over the course of three full body shiatsu treatments.
References
1. Govt. of Japan Cabinet Office website: Heisei 20 nendo-ban kokumin seikatsu akusho, 2008 (in Japanese)
2. Kober A, Scheck T, et al: Auricular acupressure as a treatment for anxiety i prehospital transport setting. Anesthesiology 98: 1328-1332, 2003
3. Sato T: Kenko na seijin josei ni okeru hando massaji no jiritsu shinkei katsudo oyobi kibun he no eikyo. Yamanashi daigaku kango gakkaishi 4(2): 25-32, 2006(in Japanese)
4. Fujita K: Haibu massaji ni yoru seijin dansei no shintaiteki • sinnriteki eikyo. Ube furontia diagaku kangogaku janaru 4(1): 37-43, 2011 (in Japanese)
5. Sakai K et al: Kenko na josei ni taisuru takutiru kea no seiriteki • shinriteki koka. Nippon kango kenkyu gakkaishi 35(1): 145-152, 2012 (in Japanese)
6. Honda Y et al: Serufu keiraku shiatsu ga kibun ni oyobosu kyusei koka to sono yuzabiriti ni kan suru kenkyu. Kenko Shien 15(1): 49-54, 2013 (in Japanese)
7. Yokoyama K: Nihongoban POMS tebiki, 1-7. Kaneko Shobo, Tokyo, 1994 (in Japanese)
8. Kamohara H et al: Effects of Shiatsu Stimulation on Peripheral Circulation. Toyo ryoho gakko kyokaishi(24): 51-56, 2002 (in Japanese)
9. Asai S et al: Effects of Shiatsu StimuIation on Muscle PIiability. Toyo ryoho gakko kyokaishi (25): 125-129, 2001 (in Japanese)
10. Yokota M et al: Effect on Pupil Diameter of Shiatsu Stimulation to the Anterior Cervical and Lateral Crural Regions. Toyo ryoho gakko kyokaishi (35): 77-80, 2011 (in Japanese)
11. Watanabe T et al: Effect on Pupil Diameter,Pulse Rate, and Blood Pressure of Shiatsu Stimulation to the Sacral Region. Toyo ryoho gakko kyokaishi (36): 15-19, 2012 (in Japanese)
12. Tadaka S et al: Tobu he no shiatsu shigeki ga doko chokkei • myakuhakusu• ketsuatsu ni oyobosu koka. Toyo ryoho gakko kyokaishi (37): 154-158, 2013 (in Japanese)
13. Kato M: Kosoku sutoresu ratto he no hari tsuden shigeki no nonai monoamin ni oyobosu eikyo. Meiji shinkyu igaku (27): 27-45, 2000 (in Japanese)